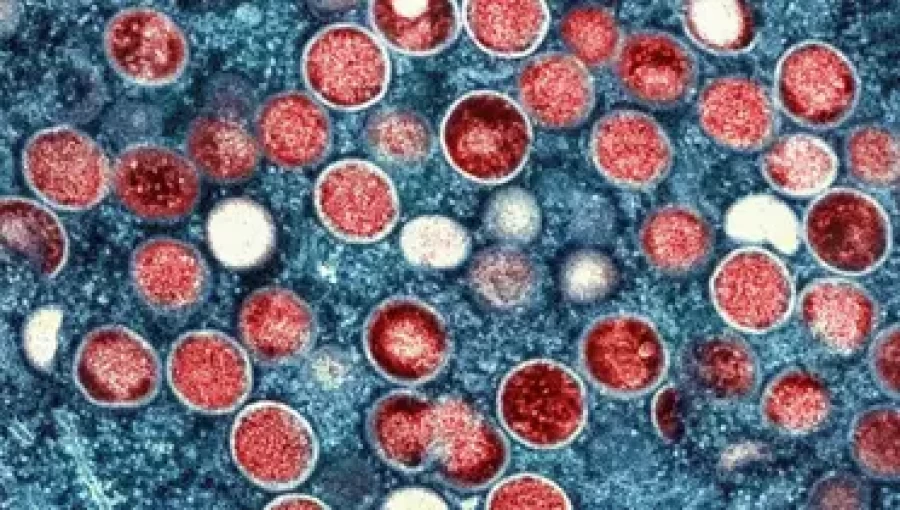
Mpox, previously known as monkeypox, has emerged as a significant global health concern, with a marked increase in cases across Africa and other regions, including Europe. This report examines the nature of mpox, its transmission pathways, symptoms, associated risks, and vital preventive measures. It highlights the current status and implications for worldwide health systems.
Understanding Mpox
Mpox is caused by the monkeypox virus (MPXV), a close relative of the smallpox virus, albeit typically less severe. Endemic to Central and West Africa, MPXV primarily circulates among wild animals but can be transmitted to humans. Since the outbreak began in 2022, cases have proliferated across multiple continents, drawing urgent global attention to this previously underreported disease.
Transmission and Spread
Mpox is transmitted through direct contact with infectious lesions, body fluids, respiratory droplets, and contaminated materials such as bedding or clothing. Human-to-human transmission occurs via close physical contact, which includes sexual interactions and prolonged face-to-face engagement. Additionally, the virus can be passed from animals to humans through bites, scratches, or handling infected wildlife.
The Democratic Republic of the Congo (DRC) faces the brunt of the outbreak, reporting over 15,000 cases and numerous fatalities in 2024 alone. Vulnerable populations, particularly children under five and individuals in conflict zones, are disproportionately affected due to crowded living conditions and limited healthcare access.
Symptoms and Risks
Symptoms of mpox typically manifest within 1 to 21 days post-exposure and can last from 2 to 4 weeks. The initial phase often resembles flu-like symptoms, including fever, headache, muscle aches, and swollen lymph nodes, followed by a distinctive rash that evolves from flat lesions to fluid-filled blisters. This rash can appear on any part of the body, including the face, hands, feet, and genital areas.
While many recover without severe complications, mpox can present serious risks for young children, pregnant women, and those with compromised immune systems. The severity of the disease varies by viral clade, with Clade I linked to higher mortality rates, particularly in African regions.
What to Do If Infected
Individuals suspecting mpox infection should seek immediate medical attention. Isolation is crucial to prevent further transmission, especially to vulnerable populations. It is advisable to cover any lesions and wear a mask when in proximity to others. Informing close contacts is essential for symptom monitoring and preventive actions.
Current treatment is supportive, aimed at alleviating symptoms and preventing complications. Vaccines, such as the JYNNEOS vaccine developed for smallpox, have demonstrated effectiveness against mpox and are recommended for those at high risk of exposure.
Global Response and Preventive Measures
The global response to mpox has intensified, featuring enhanced surveillance, public awareness campaigns, and vaccination initiatives. The World Health Organization (WHO) and other international health bodies are advocating for increased vaccine distribution, particularly in areas experiencing ongoing outbreaks. Public education on hygiene, early detection of symptoms, and safe animal handling practices are critical in mitigating the disease's spread.
In conclusion, while mpox is less transmissible than smallpox, it poses a significant public health threat due to the potential for severe outcomes, especially among vulnerable populations. Global collaboration, preventive strategies, and rapid outbreak responses are essential in addressing this urgent health challenge.
The escalating cases of mpox underscore the necessity for heightened vigilance in global health. As the disease extends beyond its traditional endemic boundaries, it is imperative that health systems worldwide remain prepared, informed, and proactive in their efforts to curb further transmission. The time for action is now.
END/DHK/RH


























Comment: